3D‐printed Engineered Trachea Functionalized by Diverse Extracellular Matrix Particles
Advanced Healthcare Materials, EarlyView.

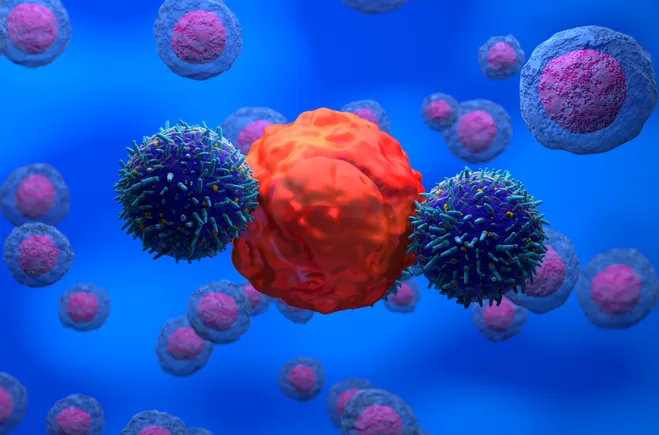
A 3D-printed engineered trachea is created using a modular strategy with decellularized extracellular matrix particles (DEPs) from costal cartilage and lungs. Costal cartilage-derived DEPs enhanced cartilage formation, while lung-derived DEPs promoted endothelial cell migration and macrophage polarization. The engineered trachea demonstrated effective vascularization and mechanical stability, showing potential for tracheal reconstruction in clinical settings.
Abstract
It remains a significant challenge to construct a tracheal substitute with both a native-like structure and multiple essential physiological functions. In this study, a combination of 3D printing techniques and a modular strategy is employed to fabricate an engineered trachea, in which the decellularized extracellular matrix particles (DEPs) from diverse sources determined specific regenerative environments in different spatial regions. Costal cartilage-derived DEPs are integrated within the cartilage rings of the engineered trachea. They effectively activated chondrocytes to secrete specific matrix proteins and develop into mature cartilage with a natural pattern of collagen deposition, which provided sufficient mechanical properties to maintain tracheal ventilation. Lung-derived DEPsare strategically placed between the cartilage rings, and are able to accelerate endothelial cell migration to form a transmural vessel network. Additionally, lung-derived DEPs exhibited a great capability to recruit macrophages and facilitate their polarization, which is beneficial for tissue regeneration. The engineered trachea underwent heterotopic vascularization and utilized for long-segmental trachea replacement in a rabbit model, demonstrating a satisfactory physiological function. Through DEP functionalization, the tracheal substitute developed a native-like complex structure with adequate mechanical supply, abundant blood perfusion, and favorable immune conditions, demonstrating significant clinical potential for patients requiring tracheal reconstruction.