This site uses cookies. By continuing to browse the site you are agreeing to our use of cookies.
All
Agriculture and Farming
Agriculture and Food News -- ScienceDaily
CropLife
Farming Today
Modern Farmer
National Sustainable Agriculture Coalition
A Reporter Gets a Buzz From Thousands of Bees
Apr 18, 2025 0
A Reporter Gets a Buzz From Thousands of Bees
Apr 18, 2025 0
Expelled From the Navy: 381 Banned Books
Apr 14, 2025 0
The Ultimate Guide to Guest Post: Boost Your ...
Mar 8, 2025 0
All
Autoblog
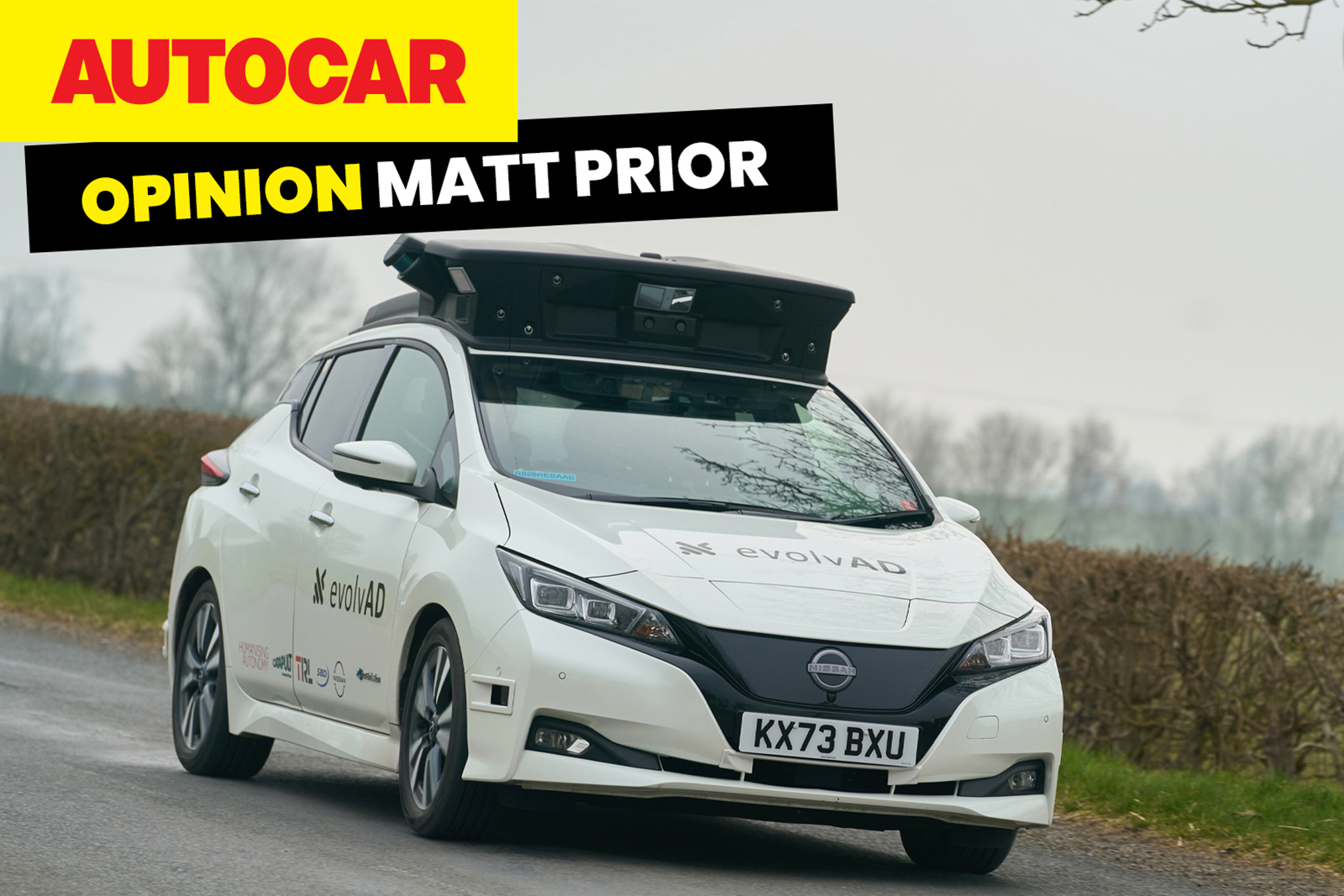
Autocar RSS Feed
Automotive News Breaking News Feed
Automotive World
Autos
Electric Cars Report
Jalopnik
Automotive News | AM-online
Speedhunters
The Truth About Cars
World premier of all-new Subaru Outback
Apr 18, 2025 0
Subaru reveals two battery electric vehicles ...
Apr 18, 2025 0
Tata Elxsi wins €50 million strategic enginee...
Apr 17, 2025 0
All
All Stories
All Stories
BioPharma Dive - Latest News
Breaking World Pharma News
Drugs.com - Clinical Trials
Drugs.com - FDA MedWatch Alerts
Drugs.com - New Drug Approvals
Drugs.com - Pharma Industry News
FDA Press Releases RSS Feed
Federal Register: Food and Drug Administration
News and press releases
Pharmaceuticals news FT.com
PharmaTimes World News
Stat
What's new
Potential Alzheimer's disease therapeuti...
Apr 13, 2025 0
New study reveals how tumors hijack key nutri...
Apr 10, 2025 0
Alternative approach to Lyme disease vaccine ...
Apr 10, 2025 0
Researchers find key to treating painful dry ...
Apr 10, 2025 0
All
Breaking DefenseFull RSS Feed – Breaking Defense
DefenceTalk
Defense One - All Content
Military Space News
NATO Latest News
The Aviationist
War is Boring
War on the Rocks
Informal meeting of NATO Ministers of Foreign...
Apr 17, 2025 0
Ceremony to mark the 70th anniversary of Germ...
Apr 17, 2025 0
Military Committee in Chiefs of Defence Session
Apr 16, 2025 0
Joint press statement
Apr 16, 2025 0
All
Advanced Energy Materials
CleanTechnica
Energy | FT
Energy | The Guardian
EnergyTrend
Nature Energy
NYT > Energy & Environment
PV-Tech
RSC - Energy Environ. Sci. latest articles
Utility Dive - Latest News
Decoding the Entropy‐Performance Relationship...
Apr 18, 2025 0
Intermetallic Electrocatalysts for Small‐Mole...
Apr 18, 2025 0
Rational Design of Carbon‐Based Electrocataly...
Apr 18, 2025 0
Smart Quasi‐Solid‐State Electrolytes with the...
Apr 18, 2025 0
Trump Opens Marine National Monument to Comme...
Apr 18, 2025 0
- Contact
- Agriculture
- Automotive
- Beauty
-
Biopharma
- All
- All Stories
- All Stories
- BioPharma Dive - Latest News
- Breaking World Pharma News
- Drugs.com - Clinical Trials
- Drugs.com - FDA MedWatch Alerts
- Drugs.com - New Drug Approvals
- Drugs.com - Pharma Industry News
- FDA Press Releases RSS Feed
- Federal Register: Food and Drug Administration
- News and press releases
- Pharmaceuticals news FT.com
- PharmaTimes World News
- Stat
- What's new
- Defense
- Energy & Water
- Fashion
- Food & Beverage
- Healthcare
- Legal
- Manufacturing
- Luxury
- Medical Devices
- Mining
- Real Estate
- Retail
- Science Journals
- Transport & Logistics
- Travel & Hospitality