Flexible Short Silica Fibers and Tricalcium Phosphate Synergistically Promote Bone Fracture Healing in Composite Cryogel Scaffolds
Advanced Healthcare Materials, EarlyView.

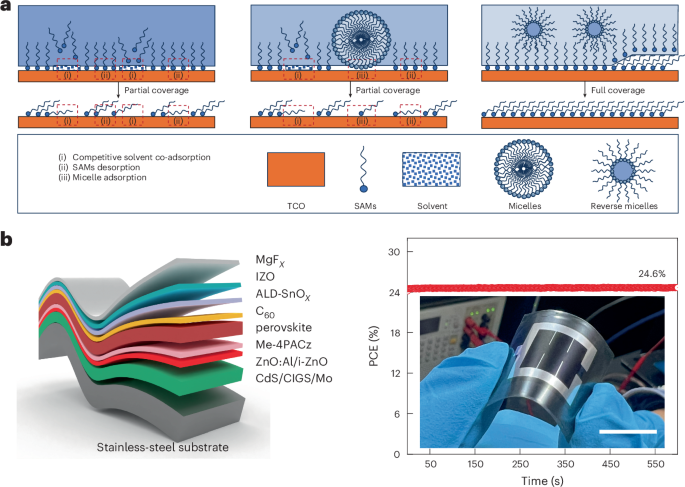
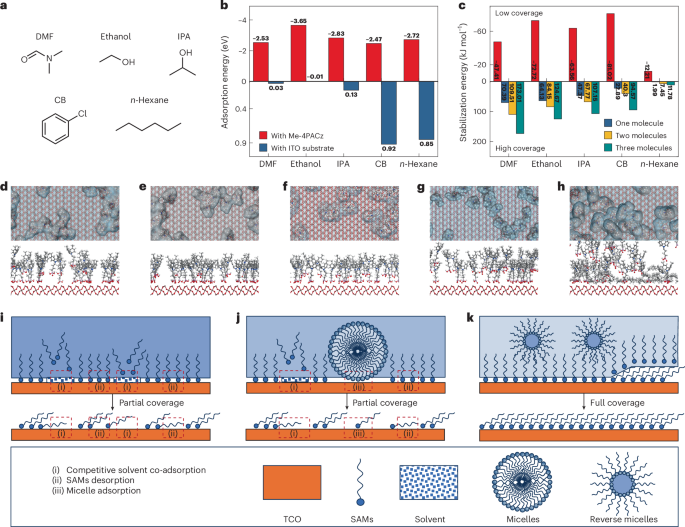
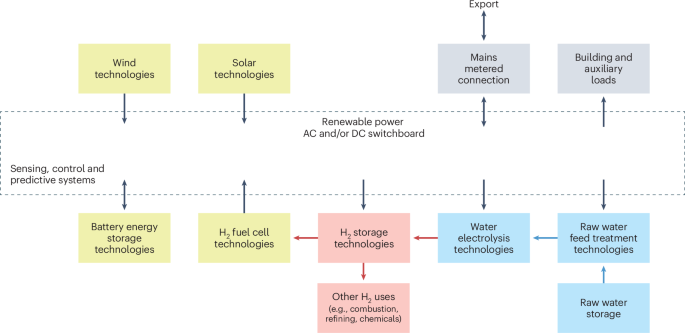
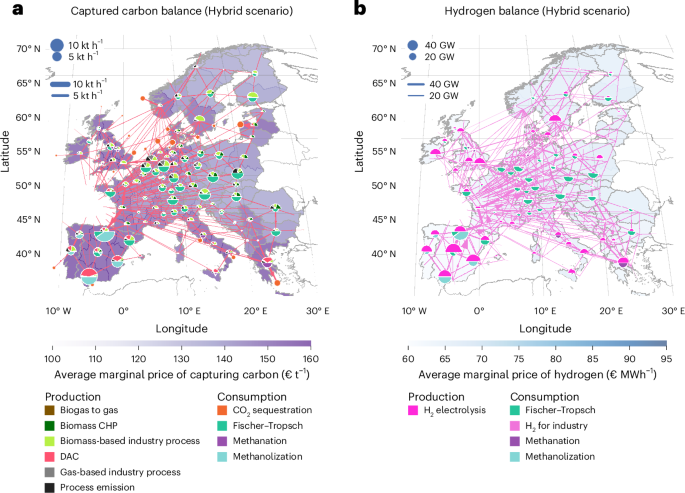
Composite cryogels combining silica fibers (SSF) and tricalcium phosphate (TCP) are fabricated via electrospinning and freeze-drying, mimicking extracellular matrix (ECM) structure and exhibiting high bioactivity. These scaffolds promoted bone healing by enhancing vascularization, mineral deposition, and bone marrow mesenchymal stem cells (BMSC) activity, supported by synergistic release ofCa2+ and Si4+ ions. in vivo assays further confirmed osteogenic potential of scaffolds, thereby offering innovative solutions for bone tissue engineering.
Abstract
Bone tissue engineering is a critical area of research focused on enhancing the regeneration of bone tissue, particularly in cases of complex defects. Despite inherent self-healing capabilities of bone, irregularly-shaped defects pose significant challenges for complete regeneration, thereby necessitating innovative therapeutic strategies. This study addresses these challenges by exploring the development of advanced tissue regeneration scaffolds. Here, tricalcium phosphate (TCP) is integrated with short silica (SiO2) fibers to develop 3D cryogel scaffolds, designated as SSFx@TCP. These cryogel scaffolds exhibit low density (<2 mg cm− 3), high water absorption (>3500%), and favorable sustained release properties, enabling effective cellular interactions. Notably, the SSFx@TCP cryogels support cell attachment, proliferation, and differentiation, while also regulate gene expression associated with angiogenesis and osteogenesis. Furthermore, in vivo assays demonstrated that these scaffolds can effectively promote de novo bone production in a rat calvarial defect model 8 weeks post-operatively, thereby indicating their potential to mimic the natural extracellular matrix. The successful integration of bioactive components in these cryogels may be beneficial for improved clinical outcomes in bone regeneration therapies and ultimately enhancing patient care in reconstructive surgery.