Extracellular Vesicles from Adipose‐Derived Mesenchymal Stem Cells Combined with PEG Hydrogel Alleviate Maternal Simulated Birth Injury in a Rat Model
Advanced Healthcare Materials, EarlyView.

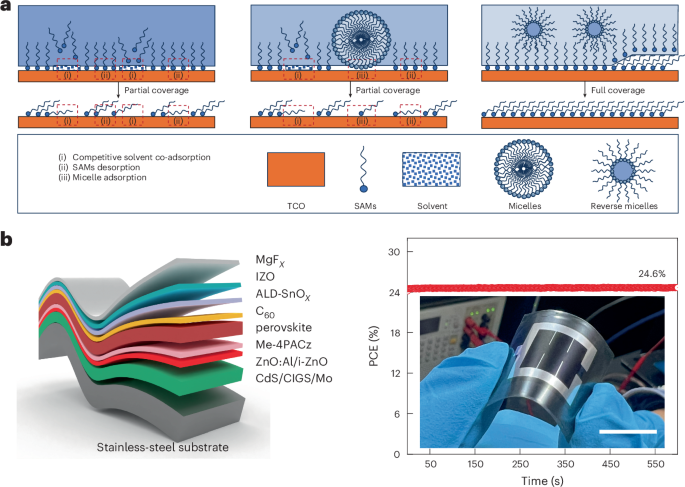
PEG@EVs promote extracellular matrix deposition by alleviating oxidative stress and ferroptosis, ultimately reducing birth-related injuries.
Abstract
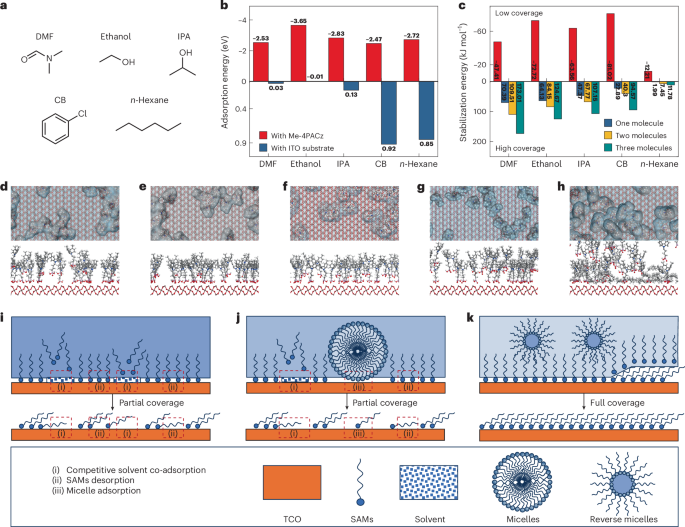
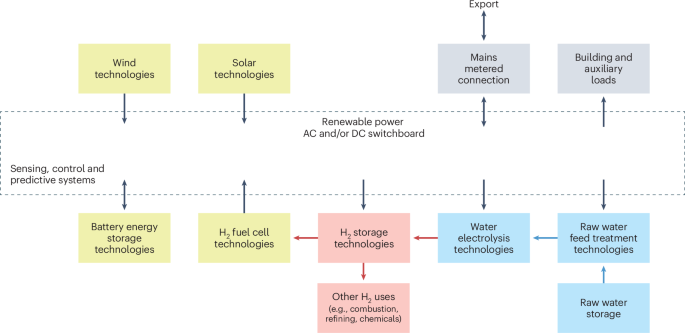
Pelvic organ prolapse (POP) is a common and distressing condition affecting women, particularly those with a history of vaginal delivery. The impact of extracellular vesicles derived from adipose-derived mesenchymal stem cells (ADSC-EVs) on pelvic floor tissue injury remains unclear. Due to their short half-life and rapid clearance in vivo, ADSC-EVs lose efficacy quickly. To address this, an injectable tetra-PEG hydrogel to encapsulate ADSC-EVs (PEG@EVs) is developed. The hydrogel is formed by tetra-PEG-NH2 and tetra-PEG-NHS through an ammonolysis reaction, leading to the formation of amide bonds within seconds. Vaginal wall tissue from POP patients shows disruption in the extracellular matrix, lipid peroxidation, and inflammation. In vitro, ADSC-EVs significantly reduce H₂O₂-induced oxidative stress, lipid oxidation, and apoptosis, while enhancing the expression of Nrf2 and its downstream targets—CAT, NQO1, HO-1, and SOD2. ADSC-EVs also upregulate GPX4 and SLC7A11, reducing mitochondrial damage and mitigating ferroptosis. The Nrf2 inhibitor ML385 reverses these protective effects. In a rat model of childbirth injury, PEG@EVs treatment promotes Nrf2 nuclear translocation, induces the M1-to-M2 macrophage conversion, reduces inflammation, and stimulates collagen deposition, thereby accelerating vaginal wall repair. The findings of this study may serve as a foundation for early targeted intervention in POP, representing a promising therapeutic approach.