Dendrimer Conjugates with PD‐L1‐Binding Peptides Enhance In Vivo Antitumor Immune Response
Advanced Healthcare Materials, EarlyView.

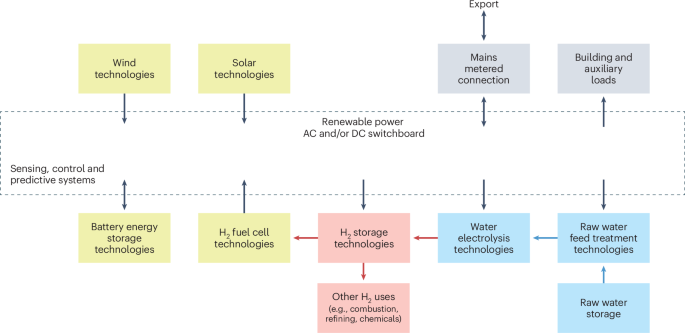
In this paper, a novel nanoparticle scaffold composed of dendrimers conjugated with peptide-based immune checkpoint inhibitors, enhancing drug delivery efficacy is introduced. By conjugating PD-L1-binding peptides to dendrimers, multivalent binding effects are harnessed, resulting in enhanced binding affinity, prolonged half-life, and improved antitumor immune responses in vivo.
Abstract
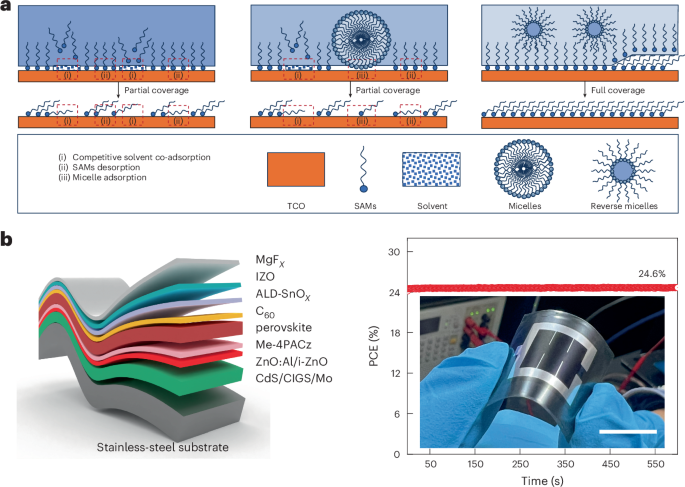
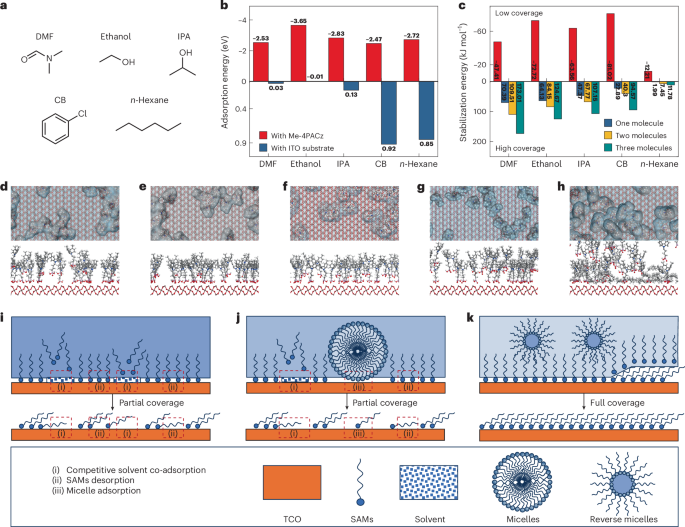
Peptides are an emerging class of biologics for cancer immunotherapy; however, their clinical translation is hindered by poor binding kinetics, bioavailability, and short plasma half-life compared to their corresponding antibodies. Nanoparticles present potential solutions but face scale-up difficulties due to complexity. Here, a translatable, modular nanoparticle scaffold is presented for peptide-based immune checkpoint inhibitors (ICIs). This platform is based on a simple structure of generation 7 (G7) poly(amidoamine) (PAMAM) dendrimers conjugated with engineered peptides (dendrimer-peptide conjugates, DPCs). DPCs functionalized with multiple copies of a programmed death-ligand 1 (PD-L1)-binding peptide exhibited significantly enhanced avidity-based binding kinetics and in vitro specificity, in addition to the substantially prolonged plasma half-life in vivo. Notably, a series of in vivo experiments revealed that DPCs displayed selective tumor accumulation and high efficacy, without apparent toxicity, when applied to a syngeneic mouse model bearing mouse oral carcinoma (MOC1) tumors. The results indicate that the DPC platform significantly improves the antagonistic effect and in vivo behaviors of the PD-L1-binding peptides, which can be potentially applied to virtually any peptide-based ICIs. The DPC platform's simplicity and modular nature will likely increase the potential of its clinical translation and ultimately enable precision/personalized cancer immunotherapy.