How Routine Medical Care Fuels America’s Opioid Crisis
By MATT McCORD When most Americans undergo surgery, they expect to recover quickly and return to their normal lives. Few realize that something as routine as a shoulder surgery, a hernia repair,Continue reading...
By MATT McCORD
When most Americans undergo surgery, they expect to recover quickly and return to their normal lives. Few realize that something as routine as a shoulder surgery, a hernia repair, or a mastectomy can mark the beginning of a life-altering opioid addiction. This often-overlooked connection between routine medical care and opioid dependence demands urgent attention.
How Physicians and Hospitals Sustain the Opioid Epidemic
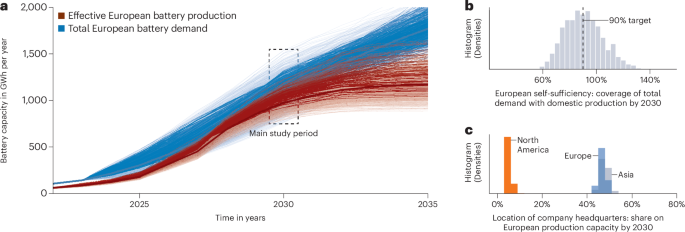
For decades, the pharmaceutical industry has shaped medical education, ingraining the belief that opioids are the best first-line treatment for acute pain. As a result, American physicians prescribe opioids at dramatically higher rates than their counterparts in other countries. A recent study in Annals of Surgery found that after three common surgeries, 91% of U.S. patients were prescribed opioids, compared to just 5% of the global patients.
Hospitals and health systems have also played a significant role in perpetuating opioid dependence. Opioids have long been a convenient and cost-effective solution for acute pain management, readily available and inexpensive to administer. However, the financial incentives for hospitals extend far beyond the initial prescription. The short-term complications of opioid use—such as nausea, constipation, urinary retention, and hyperalgesia—require additional treatments, increasing hospital revenue. Long-term complications, including dependence, overdose, and addiction, further drive profitability through repeat admissions, extended care, and emergency visits. In effect, hospitals and health systems have become financially reliant on opioid-based care, benefiting from both the immediate and prolonged consequences of opioid prescribing.
A study from the University of Michigan/IBM Watson revealed that a single opioid prescription after elective surgery increased healthcare costs by an average of $5,680 per patient per year across all payer types, including Medicare, Medicaid, and commercial insurance. This widespread cost increase affects insurance premiums, employer healthcare spending, and state and federal budgets. Notably, this estimate does not even account for the long-term costs of addiction treatment, which can be 2-16X that cost per patient per year.
The Devastating Impact of Routine Opioid Prescriptions
Each year, over 60 million surgeries are performed in the U.S., leading to the prescription of 45 million new opioid prescriptions per year. But the real crisis lies in what happens next: nearly 10% of all surgical patients remain on opioids long after their recovery should be complete. That means 2-4 million Americans every year are still using opioids beyond 90 days post-surgery.
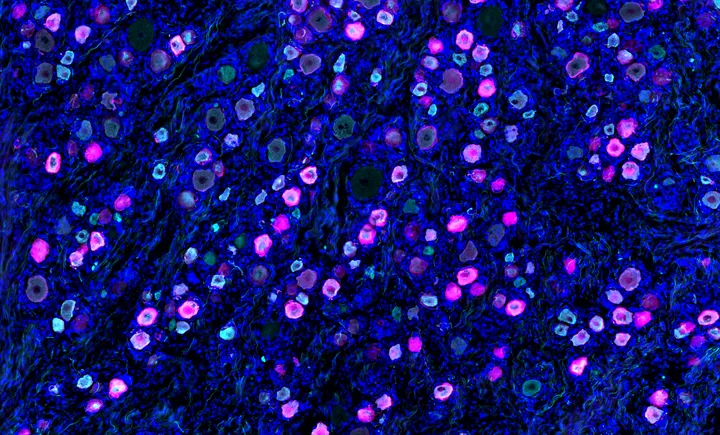
The numbers for breast cancer patients are even more staggering. A large observational study revealed that eighteen percent of women who undergo a mastectomy are still on opioids 90 days later. But for those who undergo mastectomy with reconstruction, nearly 40% remain dependent on opioids months after surgery. This is not post-operative pain; this is an opioid-induced dependency that never should have happened.
Research shows that dependence can develop within just five days of opioid use, and 14% of patients who receive a second prescription are still using opioids a year later.
Industries that demand relentless physical labor, like the Building Trades and Manufacturing, do not just expose workers to injury, they expose them to a healthcare system that routinely prescribes opioids as the default solution for pain. Every sprain, fracture, or repetitive stress injury leads these workers back into a system that feeds them the same highly addictive medications, time and time again. Opioids are not just a treatment; they become an occupational hazard. A study from Washington University in St. Louis found that 15% of construction workers prescribed opioids for musculoskeletal pain became long-term users, with those individuals being nearly 10 times more likely to develop opioid use disorder. The consequences are devastating: In 2020, the CDC reported that construction workers had an overdose death rate of 130.9 per 100,000—more than three times the national average of 41.3 per 100,000 across all industries.
The economic toll is equally staggering. The opioid crisis costs the U.S. over $1.5 trillion annually in healthcare expenses, lost productivity, and criminal justice costs. Employers alone spend more than $2.6 billion per year treating opioid addiction and overdoses. Individuals with opioid use disorder incur nearly double the annual medical expenses compared to those without the disorder.
We Need a Paradigm Shift in Acute Pain Management
Despite 72% to 88% of post-surgical patients reporting moderate-to-severe pain in the first 72 hours after surgery, opioids remain the default solution—even though they often fall short in providing effective relief and carry significant risks. Safer, more effective alternatives exist, but outdated prescribing habits and systemic barriers keep opioids entrenched in pain management.
Non-opioid alternatives for acute pain management rely on a multimodal approach that minimizes opioid exposure while effectively controlling pain—a strategy widely practiced around the world. Other high-functioning societies routinely prioritize non-opioid strategies, recognizing the dangers of opioid overuse and dependence. These alternatives include regional anesthesia techniques such as nerve blocks with long-acting local anesthetics, which provide prolonged pain relief without systemic opioid effects. Non-opioid medications like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are used in alternating schedules for continuous analgesia, while adjunctive therapies such as Gabapentinoids, intravenous lidocaine, and dexmedetomidine further enhance pain control. Non-pharmacologic interventions like cryotherapy (ice application), elevation, transcutaneous electrical nerve stimulation (TENS), mindfulness techniques, and virtual reality systems help modulate pain perception and engage the body’s natural pain-relief mechanisms. The goal should be to anchor pain management to zero opioid use whenever possible, reserving opioids only as a last resort or “break the glass” strategy when all other approaches prove insufficient. The rest of the world understands the risks of opioid use and has embraced safer, more effective alternatives—it’s time for the U.S. to follow suit.
Solutions exist, but policy and reimbursement structures must change to promote their use. Medicare has taken a step in the right direction by reimbursing non-opioid therapies outside the traditional surgical bundle, reducing financial barriers for providers. Employers and insurance carriers must follow suit, ensuring that opioid-free surgery and pain management strategies become the standard, not the exception.
Policy Recommendations for Lawmakers and Employers
To stem the opioid crisis at its source, policymakers, healthcare leaders, and employers must take immediate action:
- Remove Barriers to Surgical Alternatives – Patients should not be forced into opioid use because safer, regenerative medical treatments are inaccessible or uncovered by insurance. Expanding access to opioid-free surgical protocols and regenerative medicine can prevent long-term dependence.
- Promote Opioid-Free Surgical Outcomes – Investing in education and certification programs for both patients and providers can ensure widespread adoption of opioid-sparing strategies.
- Implement Data-Driven Accountability Measures – Health plans and hospitals should publicly report opioid prescribing patterns. Employers and insurers should incentivize opioid-free surgical options and monitor outcomes.
- Consider Clawbacks for Continued Opioid Use Beyond 90 Days – Opioid use for more than three months after an elective surgery should be treated as a complication or medical error, with financial penalties to deter excessive prescribing.
A Call to Action
We cannot solve the opioid crisis by merely reacting to prevent deaths—we must prevent addiction before it starts. While naloxone (Narcan) rescue and substance use disorder treatments are now needed in our society they do not address the underlying problem: unnecessary opioid exposure in routine medical care.
The opioid crisis often begins not in the streets, but in hospitals, doctors, and dental offices. Policymakers, employers, and healthcare leaders must act now to shift towards opioid-free acute care and long-term solutions.
Matt McCord, MD, is a practicing anesthesiologist, health benefits consultant, and cofounder of Opioid Free Solutions, which applies clinical data and best practices to reduce unnecessary opioid prescribing



























































































































































.jpg)