STAT+: UnitedHealth conducting ‘comprehensive review’ of Medicare practices that are facing federal scrutiny, new CEO says
UnitedHealth's new CEO says the company is reevaluating how it handles coding, managed care, and pharmacy services.

UnitedHealth Group’s new CEO told investors that the company is reevaluating how it tallies Medicare Advantage patients’ diagnoses for reimbursement purposes, an issue currently under investigation by the Justice Department.
Stephen Hemsley’s remarks during the company’s annual shareholder meeting on Monday signal a noteworthy shift: UnitedHealth is now publicly acknowledging potential issues with how it assesses the health of its Medicare Advantage members.
It’s a stark contrast from Hemsley’s predecessor, Andrew Witty, who pledged in April to put the gas on “engagement,” or risk adjustment coding, and blamed the government’s effort to crack down on misused codes for causing the company’s struggles. Witty stepped down the following month citing personal reasons, and the company pulled its profit outlook for the year.





















































































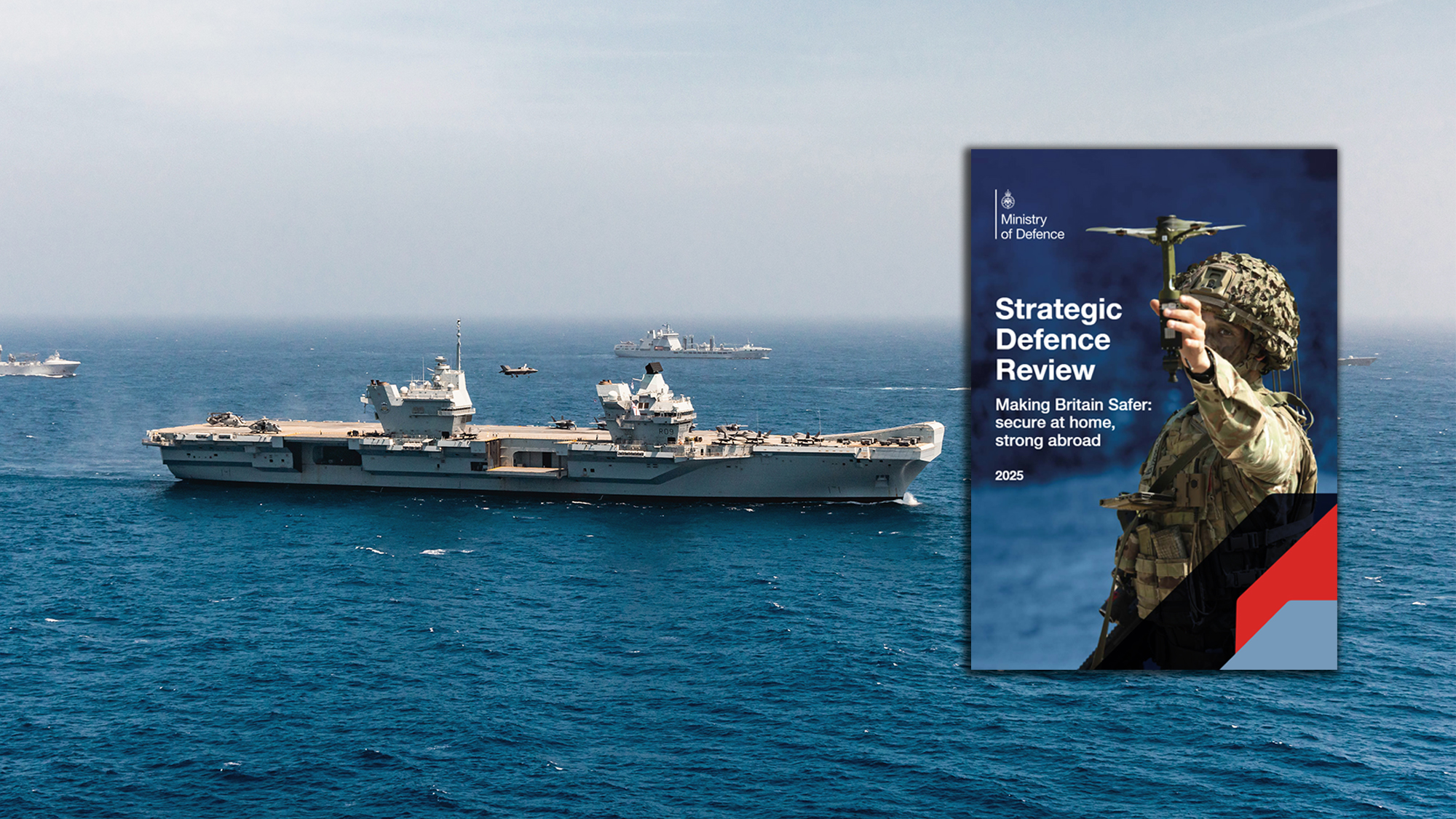
![[Video] The Weekly Break Out Ep. 20: Pacific policy in Singapore and the UK’s new defense plan](https://breakingdefense.com/wp-content/uploads/sites/3/2025/06/Break-Out-ep-20-thumb-Play-Button.jpg?#)