Short‐Chain Fatty Acids Modulate Anti‐ROR1 CAR T‐Cell Function and Exhaustion in an Intestinal Adenocarcinoma‐on‐Chip Model
Advanced Healthcare Materials, Volume 14, Issue 13, May 16, 2025.

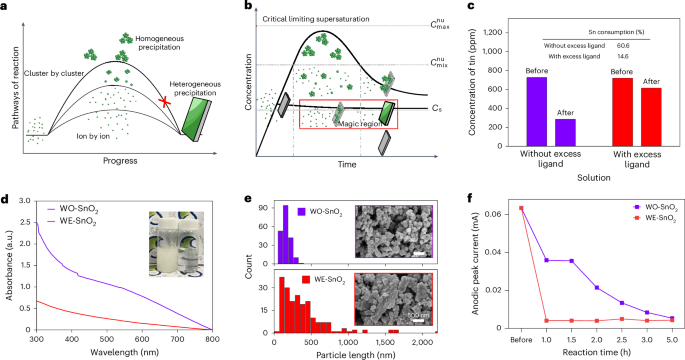
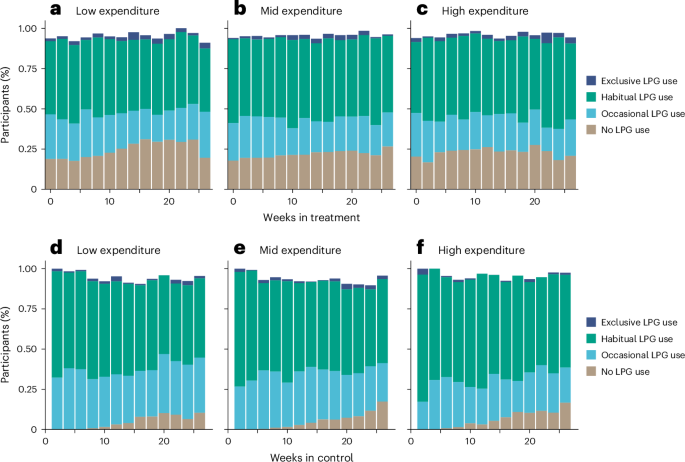
Short-chain fatty acids modulate anti-ROR1 chimeric antigen receptor (CAR) T-cell function in an intestinal adenocarcinoma-on-chip model. Butyrate and propionate reduce cytotoxicity, cytokine release, and infiltration by inducing a regulatory T-cell phenotype and T-cell exhaustion via histone deacetylase inhibition. In contrast, acetate and pentanoate support a proinflammatory Th17 phenotype, underscoring microbiota-derived metabolite influence on CAR T-cell efficacy.
Abstract
Chimeric antigen receptor (CAR) T-cell therapy represents a promising approach for cancer treatment, with receptor tyrosine kinase-like orphan receptor 1 (ROR1) emerging as a novel target in malignancies. This study investigates how short-chain fatty acids (SCFAs), key microbiota-derived metabolites, modulate anti-ROR1 CAR T-cell efficacy using a physiologically relevant intestinal adenocarcinoma-on-chip model that replicates the human intestinal microenvironment. The findings demonstrate that propionate and butyrate inhibit anti-ROR1 CAR T-cell function by reducing infiltration, cytotoxicity, and cytokine release while preserving junctional integrity within the tumor model. Mechanistically, these SCFAs inhibit histone deacetylase activity and promote a phenotype switch toward regulatory T-cells, as indicated by increased expression of FoxP3 and RORγt. Additionally, propionate and butyrate upregulate PD-1 and TIM-3, markers of T-cell exhaustion and immune tolerance, and induce a dose- and time-dependent reduction in proinflammatory cytokines. In contrast, acetate and pentanoate promote a proinflammatory T helper 17 phenotype. These results highlight the immunomodulatory effects of SCFAs on CAR T-cell function, emphasizing the need to consider microbiota-derived metabolites in CAR T-cell therapies.




























![New York City Officially Has Mechanical Garbage Trucks Now [Update]](https://www.jalopnik.com/img/gallery/new-york-city-officially-has-mechanical-garbage-trucks-now/l-intro-1749064637.jpg?#)