This site uses cookies. By continuing to browse the site you are agreeing to our use of cookies.
All
Autoblog
Autocar RSS Feed
Automotive News Breaking News Feed
Automotive World
Autos
Electric Cars Report
Jalopnik
Automotive News | AM-online
Speedhunters
The Truth About Cars
TIER IV selects PlaxidityX to provide cyber s...
May 21, 2025 0
Stellantis announces $388 million investment ...
May 21, 2025 0
NTN starts mass-production of “Resin Mold Ins...
May 21, 2025 0
Stefan Mecha becomes new Chairman of the Boar...
May 21, 2025 0
All
All Stories
All Stories
BioPharma Dive - Latest News
Breaking World Pharma News
Drugs.com - Clinical Trials
Drugs.com - FDA MedWatch Alerts
Drugs.com - New Drug Approvals
Drugs.com - Pharma Industry News
FDA Press Releases RSS Feed
Federal Register: Food and Drug Administration
News and press releases
Pharmaceuticals news FT.com
PharmaTimes World News
Stat
What's new
HER3 re-emerges as a pivotal target in the fi...
May 18, 2025 0
Drug to slow Alzheimer's well tolerated ...
May 18, 2025 0
New research offers hope for diabetic neuropa...
May 18, 2025 0
Head-to-head trial compares weight loss drugs
May 18, 2025 0
Scientific recommendations on classification ...
May 21, 2025 0
EU Implementation Guide (IG) on veterinary me...
May 21, 2025 0
All
Breaking DefenseFull RSS Feed – Breaking Defense
DefenceTalk
Defense One - All Content
Military Space News
NATO Latest News
The Aviationist
War is Boring
War on the Rocks
NATO Secretary General meets with Dutch Prime...
May 21, 2025 0
NATO Secretary General commends Czechia’s com...
May 21, 2025 0
Secretary General calls for stronger NATO-EU ...
May 20, 2025 0
NATO Secretary General meets the Minister of ...
May 20, 2025 0
All
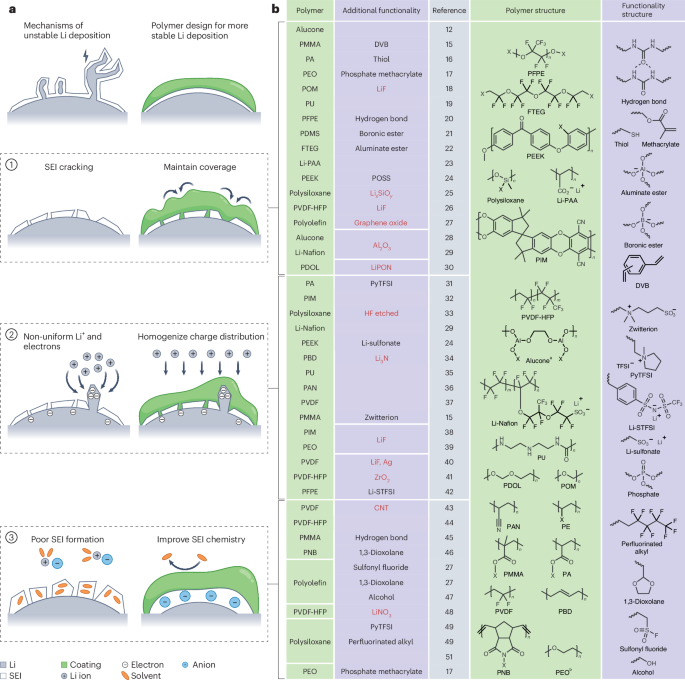
Advanced Energy Materials
CleanTechnica
Energy | FT
Energy | The Guardian
EnergyTrend
Nature Energy
NYT > Energy & Environment
PV-Tech
RSC - Energy Environ. Sci. latest articles
Utility Dive - Latest News
Protonated Pyridinic Nitrogen Enhances Chlori...
May 21, 2025 0
Crosslinked Conjugated Interlayer Network for...
May 20, 2025 0
Tuning Anion Chemistry to Enhance Bulk and In...
May 20, 2025 0
Green‐Solvent‐Processed Scalable Semi‐Transpa...
May 20, 2025 0
Author Correction: US industrial policy may r...
May 19, 2025 0
- Contact
- LIVE TV
- Agriculture
- Automotive
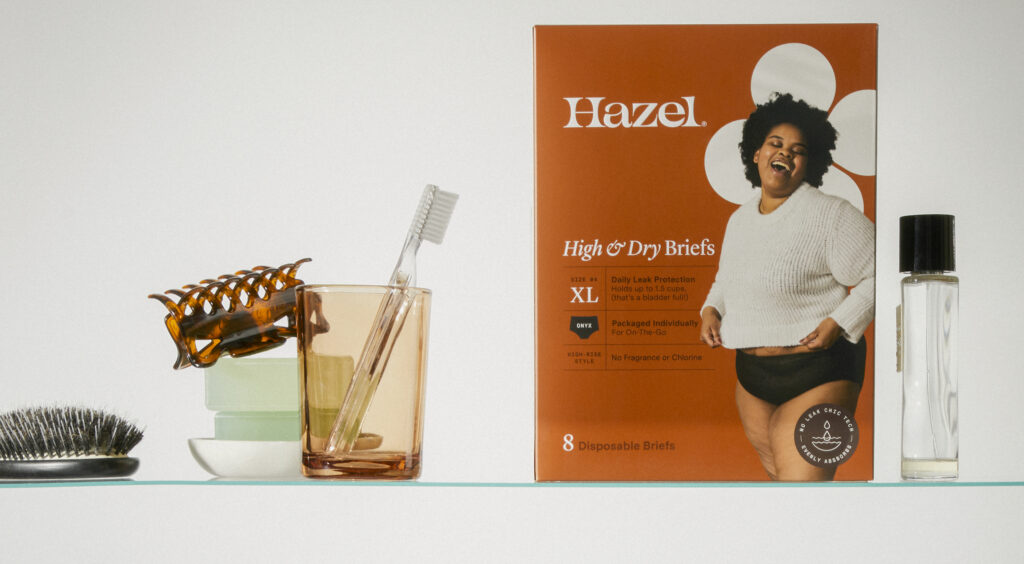
- Beauty
-
Biopharma
- All
- All Stories
- All Stories
- BioPharma Dive - Latest News
- Breaking World Pharma News
- Drugs.com - Clinical Trials
- Drugs.com - FDA MedWatch Alerts
- Drugs.com - New Drug Approvals
- Drugs.com - Pharma Industry News
- FDA Press Releases RSS Feed
- Federal Register: Food and Drug Administration
- News and press releases
- Pharmaceuticals news FT.com
- PharmaTimes World News
- Stat
- What's new
- Defense
- Energy & Water
- Fashion
- Food & Beverage
- Healthcare
- Legal
- Manufacturing
- Luxury
- Medical Devices
- Mining
- Real Estate
- Retail
- Science Journals
- Transport & Logistics
- Travel & Hospitality