Can EHRs Expand to Become Health Systems’ “Platform of Platforms” (UDHPs)?
By VINCE KURAITIS & NEIL JENNINGS In a previous post in this series, we discussed healthcare’s migration toward Unified Digital Health Platforms (UDHPs) — a “platform of platforms.” Think of a UDHP asContinue reading...



In a previous post in this series, we discussed healthcare’s migration toward Unified Digital Health Platforms (UDHPs) — a “platform of platforms.” Think of a UDHP as healthcare’s version of a Swiss Army knife: flexible, multi-functional, and (ideally) much better integrated than the drawer full of barely-used apps most health systems currently rely on. We included a list of 20+ companies jockeying for UDHP dominance, including two familiar EHR (electronic health record) giants — Epic and Oracle. This raises the obvious question for today’s post:
Can EHRs level up into becoming UDHPs — becoming healthcare’s platform of platforms? Or are they trying to wear a superhero cape while tripping over their own cables?
We see good arguments pro and con, and like most things in healthcare “it’s complicated.” Some say EHRs are uniquely positioned to make the leap. Others believe the idea is like trying to teach your fax machine to run population health analytics.
Thus, we’ll lay out the arguments for differing points of view, and you can decide for yourself.

by Vince Kuraitis and Neil P. Jennings of Untangle Health
Here’s an outline of today’s blog post:
- A Brief Recap: What are UDHPs?
- Thesis: EHRs Can Expand to Become UDHPs
- EHRs Currently Own the Customer Relationship
- Many Customers Have an “EHR-First” Preference for New Applications
- Epic and Oracle Health are Making Strong Movements Toward Becoming UDHPs
- Antithesis: EHRs Can NOT Become Effective EHRs
- EHRs Carry a Lot of Baggage
- Customers are Skeptical
- EHR Analytics Are NOT Optimized To Achieve Critical Health System Objectives
- EHR Switching Costs are Diminishing
- Cloud Native Platforms Accelerate Innovation and Performance
- It’s Not in EHR DNA to Become A Broad-Based Platform
- Synthesis and Conclusion
This is a long post…over 4,000 words…so we’ve clearly got a lot to say on the matter. Hope you brought snacks!
A Brief Recap: What are UDHPs? (Unified Digital Health Platforms)
In our previous extensive post on UDHPs, we described them as a new category of enterprise software. A December 2022 Gartner Market Guide report characterized the long-term potential:
The [U]DHP shift will emerge as the most cost-effective and technically efficient way to scale new digital capabilities within and across health ecosystems and will, over time, replace the dominant era of the monolithic electronic health record (EHR).
The DHP Reference Architecture is illustrated in a blog post by Better. Note that UDHPs are visually depicted as “sitting on top” of EHRs and other siloed sources of health data:

We noted that almost any type of large healthcare organization — health systems, health plans, pharma companies, medical device companies, etc. — had a need for UDHPs. However, today’s focus is more narrow — we limit the discussion to UDHPs in hospitals and health systems, primarily in the U.S. We use the term “health system” to encompass hospitals and regional health delivery systems.
In this post, we focus on the two largest EHR vendors in the U.S. — Epic and Oracle Health; they have a combined market share of 65% of hospitals and 77% of hospital beds.
In the remaining sections, we will lay out arguments on both sides of the issue of whether EHRs can (or cannot) expand to become UDHPs. The graphic below is our crack at a visual summary. The balloons represent the thesis – that EHRs can expand to become UDHPs; the anchors represent the antithesis – that EHRs can not expand to become UDHPs.


Thesis: EHRs Can Expand To Becoming UDHPs
Let’s look at the case for EHRs expanding to become effective UDHPs.
1) EHRs Currently Own the Customer Relationship
Fueled by federal HITECH incentives and mandates, health systems have made significant investments in their existing EHRs:
- As of 2021, 96% of non-federal acute care hospitals in the U.S. had adopted a certified EHR.
- They made huge capital commitments to purchase and install their EHR, often hundreds of millions of dollars.
- Many existing clinical workflows are built on EHRs.
- A majority of a patient’s clinical data in a health system resides inside their EHR.
According to SoftwareReviews, Epic and (Oracle) Cerner Millennium EHRs receive good to high ratings from health system customers.
Thus, any new vendor attempting to sell new healthcare enterprise software (i.e., a UDHP) will face a high hurdle: “We already have an EHR…why should we consider you?”
2) Many Customers Have an “EHR-First” Preference for New Applications
Health systems have been trying to stay afloat in a veritable tsunami of point solutions. This creates a range of challenges, including:
- Complexity and integration challenges
- Regulatory and compliance risks
- Fragmentation of care
- User adoption and training
- Cost and ROI concerns
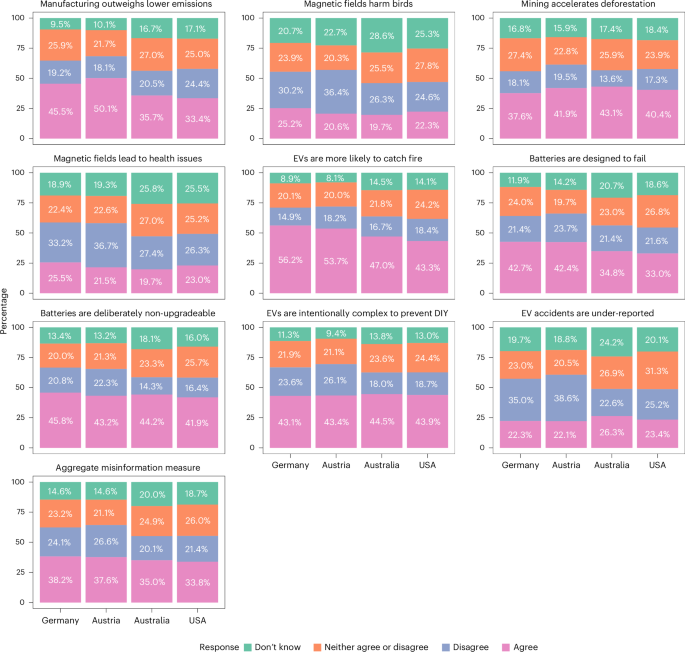
As shown in the graphic below, a 2024 Bain & Company/KLAS survey of health systems found that 81% increasingly plan to look to existing vendors before considering offerings from new vendors.
More specifically, the survey found that 79% plan to look to their EHR vendor first for new solutions before looking to others.

University Hospitals is an example of a health system with an EHR-First strategy. According to Robert Eardley, CIO, this guiding principle ensures the health system prioritizes tools and innovations available within its Epic electronic health record platform whenever feasible.
3) Epic and Oracle Are Making Strong Movements Toward Becoming UDHPs
Perhaps the best argument that EHRs are capable of becoming Unified Digital Health Platforms is that Epic and Oracle Health are already making bold moves. Let’s take a look at them individually.
Epic’s EHR Expansion Plans
Epic is more than a basic EHR — it offers existing customers a broad base of capabilities. Interop guru Brendan Keeler has written extensively about Epic. In his article “An Epic Saga: The Origin Story” he describes how Epic grew to its current size. The Appendix provides an extensive list of “Epic Modules.”
In an insightful 2024 analysis of Epic’s dominant market position, Seth Joseph included a list of Products You Can Replace with Epic. The list included over 150 capabilities “to help you identify areas where you could use your Epic software to either replace or avoid purchasing niche applications…”
 Epic also is expanding new offerings to new customer categories. In the article “Epic Beyond the Provider Empire“, Brendan Keeler provides a detailed list:
Epic also is expanding new offerings to new customer categories. In the article “Epic Beyond the Provider Empire“, Brendan Keeler provides a detailed list:
 Health Grid — software sold to
Health Grid — software sold to
- Labs
- Medical device companies
- Payers
- Telehealth companies
- Clinical trials
Health Grid Adjacent offerings
- Cosmos — “a massive clinical dataset created by pooling information from Epic health systems”
- Payer Gateway — a “lighter-weight service for payers that enables them to receive clinical data from Epic healthcare organizations”
- Chart Gateway — “Epic’s service that streamlines how life insurance companies get medical records from Epic healthcare organizations”
- EpicCare Link — “a web-based portal product that lets Epic healthcare organizations offer non-Epic providers a way to interact with them.”
Other stuff
- Supply Shop — services offerings
- Revcyclers — “Third parties working with Epic and provide billing services to help improve revenue cycle outcomes”
- Cornerstone Partners — deep relationships with Microsoft and InterSystems
But wait…there’s more. At HIMSS 2025, Epic announced additional AI capabilities in the works and that it is developing a healthcare-specific enterprise resource planning (ERP) system. While we view an ERP as a big stretch, it’s also a potential game-changer for Epic.
Using a framework created by David Yuan of Tidemark, Brendan Keeler capsulized Epic’s broader platform strategy:
With additions like the ERP, Epic is clearly evolving beyond a traditional EHR system, but is it enough to meet the UDHP needs of modern health systems?
Oracle Health Goes Beyond Being a Traditional EHR
In October 2024, Oracle announced a new EHR. As described by the company, Oracle Health has many characteristics that make it look more like a UDHP than a traditional EHR. It aims to go significantly beyond the capabilities of a traditional EHR:
- Embedded Artificial Intelligence (AI): Unlike EHRs where AI is often a bolt-on, Oracle’s new system is designed with AI as a core component, integrated across the entire clinical workflow. This includes a Clinical AI Agent, AI-driven insights at the point of care, AI-powered summaries, and personalized care plans.
- Enhanced User Experience: Recognizing the clinician burden associated with traditional EHRs, the new system emphasizes an intuitive and user-friendly design with features like voice-driven navigation and search, multimodal search, and a customizable interface.
- Oracle Health Data Intelligence is an AI and analytics solution embedded within the EHR, enabling integration of disparate data sources, real-time insights, and population health management tools.
- Next-Generation Oracle Cloud Infrastructure offers advantages of enhanced security, scalability, and performance, and better data exchange.
- Patient Engagement Tools: The new EHR includes a reimagined patient portal focused on empowering patients to access and control their medical history, facilitating communication with providers, and enabling self-service capabilities for patients to manage appointments, pay bills, and access health information.
- Focus on Value-Based Care: The system is designed to support value-based care models by streamlining information exchange between payers and providers, improving care coordination, and providing insights into cost and resource allocation.
Oracle Health aims to move beyond being a system of record to becoming a system of action — an intelligent, integrated platform that actively assists clinicians, engages patients, and drives better outcomes in a more efficient and secure manner. Oracle’s most recent announcement of a platform partnership with Cleveland Clinic and G42 is consistent with the migration toward becoming a UDHP.
Oracle Health is still in its early stages of a roll-out, with an early adopter program launched in 2025. Therefore, extensive, widely published surveys and large-scale customer feedback about this new platform aren’t yet available.
Antithesis: EHRs Can NOT Become Effective UDHPs
Now let’s examine arguments suggesting that EHRs aren’t capable of becoming health systems’ “platform of platforms” — a UDHP.
1) EHRs Carry a Lot of Baggage
Today’s EHRs are criticized on a number of fronts: errors and safety issues, cost, lack of competition, lack of interoperability, and lack of usability for clinicians. COVID-19 highlighted many of the weaknesses in EHRs as being “large, slow monoliths that don’t quickly adapt to new, emergent demands on their design and workflow.”
But what about the high satisfaction scores previously cited? EHRs are more likely to consider health system administrators as their “customers.” As noted above, clinician “user” satisfaction is generally low.
Vendors also have allowed customers to customize EHR implementations. Local customization leads to substantial differences in how the system operates from one site to another. The often-used colloquial phrase is that there are “50 dialects of Epic.” While some degree of EHR customization is necessary and can increase clinician buy-in, over-customization can result in difficulty interoperating, as data definitions and workflows can differ greatly. With each EHR instance potentially unique, extending EHRs to become UDHPs carries forward organization-specific configurations which may result in substantial longitudinal maintenance (for either the health system or the partners connected to the EHR).
Finally, Epic’s unique size and dominant market position could attract antitrust challenges from government regulators. Even today, as Seth Joseph documents, Epic is already attracting lawsuits from multiple “smaller, adjacent vendors.” As Epic adds ERP and Cerner and Epic continue adding adjacent features and capabilities, they are expanding their positions, potentially garnering additional regulatory oversight.
2) Customers are Skeptical
 Even while many health systems might have an “EHR-First” integration preference, many are also skeptical of their EHR vendor’s promises and their ability to integrate new apps. Sage Growth Partners report entitled The New Healthcare C-Suite Agenda: 2024-25 addressed the issue:
Even while many health systems might have an “EHR-First” integration preference, many are also skeptical of their EHR vendor’s promises and their ability to integrate new apps. Sage Growth Partners report entitled The New Healthcare C-Suite Agenda: 2024-25 addressed the issue:
C-Suites are at a technology crossroads: Very few are satisfied with their EMR vendor, the market is flooded with point solutions but integrations are frustrating employees more, and despite the policy relaxations around telehealth during the last three years, telehealth and in-home hospital tools are not well integrated with EMRs.
When asked “How well does your current vendor live up to the promises it makes about the EMR, only 26% responded “extremely well” or “very well.”
Perhaps most importantly, “