Cascade‐Responsive Nanoprodrug Disrupts Immune‐Fibroblast Communications for Potentiated Cancer Mechanoimmunotherapy
Advanced Healthcare Materials, Volume 14, Issue 11, April 25, 2025.

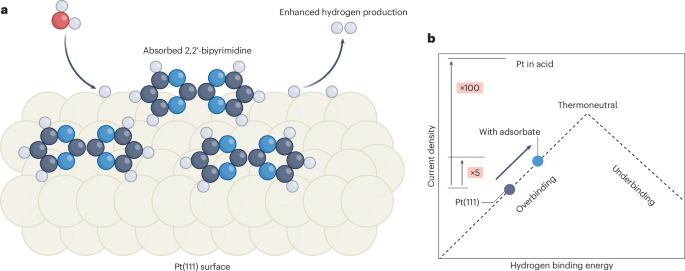
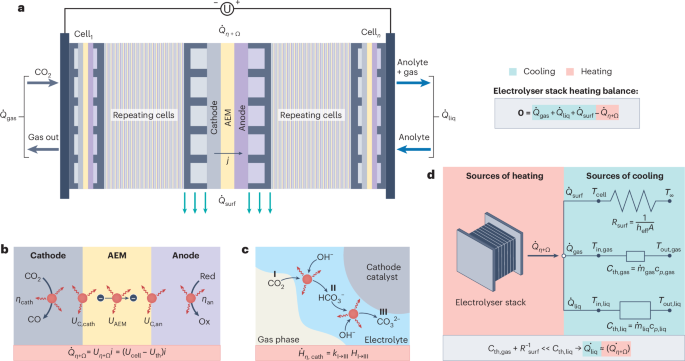
Herein, this study demonstrates that FAP-α+CAFs-induced stromal stiffness accelerated tumor progression by precluding cytotoxic T lymphocytes. Subsequently, a cascade-responsive nanoprodrug capable of re-educating FAP-α+CAFs and amplifying tumor immunogenicity is constructed. Benefiting from the disruption of immune-fibroblast communications, this mechanoimmunotherapy strategy rekindles immune response to inhibit triple-negative breast cancer growth and metastasis, providing a novel sight for desmoplastic cancer treatment.
Abstract
The abnormal tumor mechanical microenvironment due to specific cancer-associated fibroblasts (CAFs) subset and low tumor immunogenicity caused by inefficient conversion of active chemotherapeutic agents are two key obstacles that impede patients with desmoplastic tumors from achieving stable and complete immune responses. Herein, it is demonstrated that FAP-α+CAFs-induced stromal stiffness accelerated tumor progression by precluding cytotoxic T lymphocytes. Subsequently, a cascade-responsive nanoprodrug capable of re-educating FAP-α+CAFs and amplifying tumor immunogenicity for potentiated cancer mechanoimmunotherapy is ingeniously designed. Benefiting from the active targeted release of angiotensin II receptor antagonist (losartan) guided by FAP-α cleavable peptide and the efficient conversion of topoisomerase I inhibitor (7-Ethyl-10-hydroxycamptothecin) prodrug under high glutathione/esterase within tumor cells, this regimen created an immune-activated landscape that retarded primary tumor growth and counteracted resistance to immune checkpoint inhibitor in mice with triple-negative breast cancer. This nanoprodrug-assisted mechanoimmunotherapy can serve as a universal strategy for conferring efficient tumoricidal immunity in “immune excluded” desmoplastic tumor interventions.